Cardiac arrest is a critical medical emergency characterized by the sudden cessation of effective cardiac function, leading to the loss of circulation and subsequent organ failure. It is imperative for healthcare professionals, particularly those involved in Advanced Cardiac Life Support (ACLS), to recognize the signs and symptoms of cardiac arrest swiftly and accurately. Patients experiencing cardiac arrest may present with unresponsiveness, absence of normal breathing, and lack of a palpable pulse. These clinical indicators necessitate immediate intervention, as the likelihood of survival decreases significantly with each passing minute without proper resuscitation efforts.
The underlying causes of cardiac arrest can be diverse, ranging from cardiac arrhythmias, myocardial infarction, and severe electrolyte imbalances to non-cardiac factors such as trauma, respiratory failure, or drug overdose. Understanding the etiology is crucial for effective management and treatment. In many cases, the primary rhythm observed during cardiac arrest is either ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT), both of which require rapid defibrillation as part of the initial resuscitation efforts. Additionally, the recognition of potential reversible causes, often summarized as the “Hs and Ts†(hypovolemia, hypoxia, hydrogen ion accumulation, hyper/hypokalemia, hypothermia, tension pneumothorax, cardiac tamponade, toxins, thrombosis), can direct appropriate therapeutic interventions.
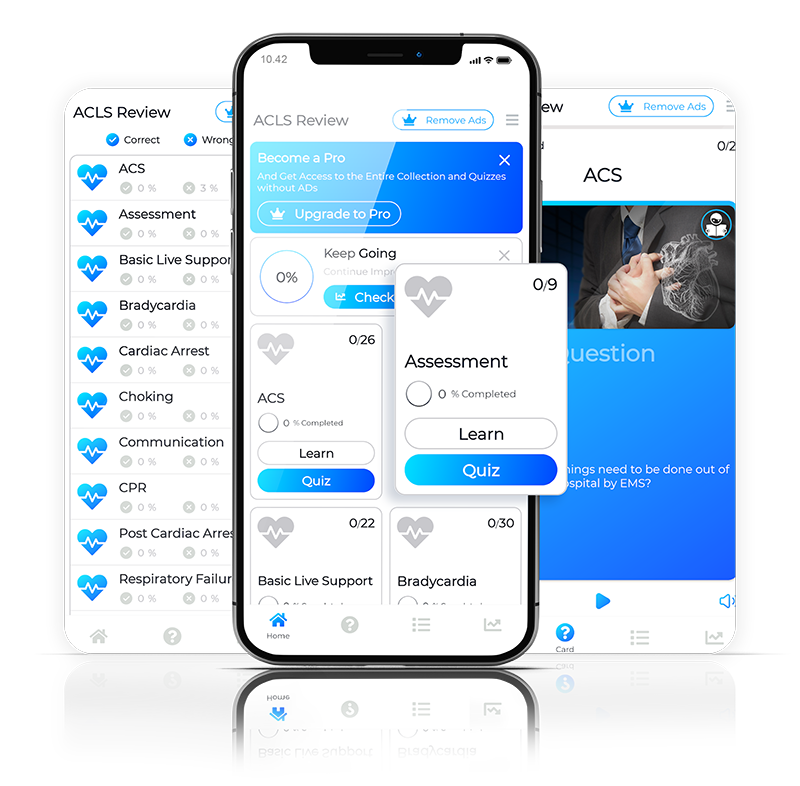
ACLS protocols emphasize the importance of high-quality cardiopulmonary resuscitation (CPR) in the early management of cardiac arrest. High-quality CPR includes ensuring adequate chest compressions at the recommended rate and depth, minimizing interruptions, and providing appropriate ventilations. The use of an automated external defibrillator (AED) should be prioritized as soon as it becomes available. Healthcare providers get more info should be familiar with the ACLS algorithms that guide the differential treatment of cardiac arrest based on the presenting rhythm, emphasizing the need for timely and effective rhythm analysis, defibrillation, and post-resuscitation care.
Post-cardiac arrest care is equally critical and involves stabilization of the patient, identification of the underlying cause, and monitoring for potential complications. Therapeutic hypothermia, when indicated, has been shown to improve neurological outcomes in patients who remain comatose after return of spontaneous circulation (ROSC). Continuous evaluation and adjustment of treatment strategies based on the patient's response are essential, as is collaboration among the multidisciplinary team to ensure comprehensive care. The recognition of signs indicating a favorable or unfavorable prognosis post-resuscitation can guide further interventions and discussions with family members regarding the patient's future care.
In conclusion, cardiac arrest remains a significant challenge in the field of emergency medicine, demanding urgency and precision from healthcare professionals. Mastery of ACLS algorithms, alongside a robust understanding of the pathophysiology of cardiac arrest, is essential for optimizing patient outcomes. Continuous education and simulation training are vital for maintaining competency in resuscitation techniques, enabling healthcare providers to respond effectively to this life-threatening condition. Through a combination of prompt recognition, high-quality CPR, and appropriate post-resuscitation care, healthcare professionals can enhance survival rates and improve the quality of life for patients who experience cardiac arrest.